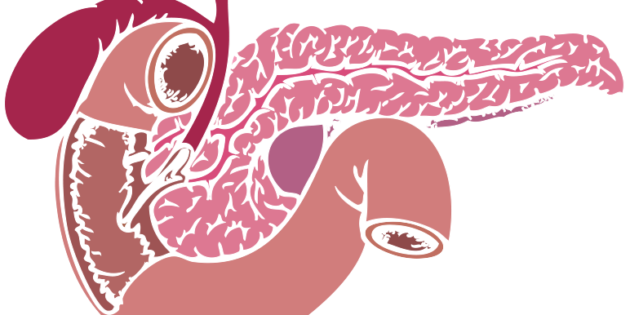
The pancreas is a multitasking organ. Unlike other organs, it functions as an exocrine and endocrine gland, meaning that its secretions will reach the blood either directly or through a vessel. Its exocrine function includes the production of enzymes that help with digestion. And its endocrine function is to release hormones that control blood sugar levels.
The pancreas is crucial to healthy digestion. If the pancreas produces low-quality or insufficient digestive enzymes, the body will not digest foods or absorb nutrients properly. If the pancreas does not make enough of the hormones insulin, glucagon, or somatostatin, then blood sugar levels will not be balanced, and feelings of lack of energy will rise due to improper absorption processes.
Common problems with the pancreas include:
- Exocrine and endocrine pancreatic insufficiency.
- Inflammation of the pancreas (pancreatitis).
- Pancreatic cancer.
You will feel that you have problems with your pancreas when you have chronic upper abdominal pain that worsens after food and may radiate to your backside. The pancreas area will feel tender upon touching. Your stools will be fatty, and you may suffer from vomiting bouts, fever, and rapid heart rate. You may also notice sudden weight loss due to malnutrition.
Here are some natural ways to improve pancreas health and function:
Remove alcohol from the diet
In the majority of pancreatitis cases, alcohol use was the cause. [1] In chronic pancreatitis, alcohol consumption may lead to the condition much sooner than the development of alcohol-induced liver cirrhosis. There is no need for long-term alcohol consumption to cause pancreas destruction. [2-3]
When you drink alcohol, your pancreas metabolizes the alcohol, and the toxic byproducts damage your pancreatic ducts, and healthy enzyme release is impacted. Instead of enzymes that break down the food being released into your digestive tract, they build up and begin to digest your pancreas instead. This leads to damage of pancreatic tissues leading to inflammation. Alcohol consumption also leads to nutrient displacement, another risk factor for poor pancreatic function, as I will discuss later.
Watch protein intake
Research studies report that patients with chronic pancreatitis consumed higher protein intakes than healthy controls. [4-7]
The risk of developing chronic pancreatitis was shown to increase depending on the quantity of consumed protein, and alcohol. [8]
Thus, it is crucial to consume protein within the healthy range of 0.8 grams per kilogram of body weight.
Micronutrient intake
Studies have shown that people with chronic pancreatitis have nutrient deficiencies. [9-11]. This is especially true in the case of high caloric intake with little nutritive value, as this will exacerbate nutritional deficiencies. Nutritional deficiencies will negatively affect the outcome of the disease if they are not treated on time. Therefore, I recommend supplementing your diet with methyl donor nutrients, including:
- B-complex three times a week
- Vitamin B12 in the form of methylcobalamin once a week.
And consuming foods rich in:
The amino acid methionine (brazil nuts, soybeans, tofu, beans, lentils, wheat germ, and spirulina)
Betaine (quinoa, beets, spinach, and amaranth
Zinc (legumes, nuts, seeds, and whole grains).
Red meat intake
Red and processed meat consumption are related to pancreatic cancer. A meta-analysis showed a significantly increased risk of pancreatic cancer with red meat consumption, especially barbecued meat consumption. [12-15]
High meat cooking temperatures are also related to pancreatic cancer through increased production of glycation end products (AGEs) and heterocyclic amines, contributing to insulin resistance, oxidative stress, chronic inflammation, and pancreatic cancer. [13, 16-20].
Other studies reported that people with chronic pancreatitis consumed more animal-based protein than controls. [21, 13]
Another study showed that red meat intake was associated with recurrent acute or chronic pancreatitis across all ethnic groups, and dietary fiber protected against acute pancreatitis.[22]
I recommend reducing all meat consumption to support pancreatic health. Preferably have the protein come from plant-based sources such as lentils (cooked, not dried), soy, leafy green vegetables, and broccoli.
Digestive enzyme supplements
You can also support pancreatic health issues with digestive enzyme supplementation. Pancreatin is a combination of digestive enzymes necessary for digesting fats, proteins, and sugars. The pancreas typically produces these. According to a study, enzyme supplementation can play an integral role in digestive disorders and treat pancreatic insufficiency. [23-24]
Many pancreatin supplements on the market contain bromelain, pancreatic enzymes, and peptidases to help digest food more effectively.
Choose the right hydration
Increasing fluid intake is crucial to pancreatic health. Water is key. On the other hand, do not drink fruit juices as they become higher in sugar through the blending process that may impact pancreatic health. If you have a weak pancreatic function, you may already be prediabetic or diabetic. Therefore, you should avoid any sugary drinks, including natural fruit juices.
A somewhat healthier alternative would be fresh vegetable juices made with anti-inflammatory leafy greens such as kale, spinach, chard, dandelion leaves, parsley, cilantro, and oregano without any added fruits. Dark leafy greens are rich in antioxidants, while cruciferous vegetables such as broccoli, Brussels sprouts, and cabbages are high in fiber, vitamin C, vitamin K, and sulforaphane. Cucumber and celery combined are excellent juices to include in your diet for detoxification and healing purposes.
Feel free to comment below and let me know what you liked best about this article.
Thank you for taking the time to read this. I’d be honored if you would share it with your family, friends, and followers by clicking the Like, Tweet, and Share buttons. If you are serious about improving your health no matter what your age or circumstances, and are ready to finally achieve optimal health and lose the weight you’ve been struggling with, then click HERE to check out my online Guerrilla Diet Wholistic Lifestyle Bootcamp for Healthy and Lasting Weight Loss.
If you are not already on my mailing list where you will receive my weekly articles packed with scientifically based health, and nutrition content, as well as many FREE bonuses and special offers, and much more, then click HEREto subscribe.
Thank You, 🙂
Dr. Galit Goldfarb
References
- Gapp J, Chandra S. Acute Pancreatitis. [Updated 2021 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Lévy P, Mathurin P, Roqueplo A, Rueff B, Bernades P. A multidimensional case-control study of dietary, alcohol, and tobacco habits in alcoholic men with chronic pancreatitis. Pancreas. 1995;10:231–238.
- Durbec JP, Sarles H. Multicenter survey of the etiology of pancreatic diseases. Relationship between the relative risk of developing chronic pancreaitis and alcohol, protein and lipid consumption. Digestion. 1978;18:337–350
- Uscanga L, Robles-Díaz G, Sarles H. Nutritional data and etiology of chronic pancreatitis in Mexico. Dig Dis Sci. 1985;30:110–113.
- Laugier R, Bernard JP, Laroche R, Kadende P, N’Dabaneze E, Saunière JF, Dupuy P. Exocrine pancreatic secretion in normal controls and chronic calcifying pancreatitis patients from Burundi: possible dietary influences. Digestion. 1993;54:54–60.
- Noel-Jorand MC, Bras J. A comparison of nutritional profiles of patients with alcohol-related pancreatitis and cirrhosis. Alcohol Alcohol. 1994;29:65–74
- Dani R, Mott CB, Guarita DR, Nogueira CE. Epidemiology and etiology of chronic pancreatitis in Brazil: a tale of two cities. Pancreas. 1990;5:474–478
- Durbec JP, Sarles H. Multicenter survey of the etiology of pancreatic diseases. Relationship between the relative risk of developing chronic pancreaitis and alcohol, protein and lipid consumption. Digestion. 1978;18:337–350.
- Bao Y., Michaud D.S., Spiegelman D., Albanes D., Anderson K.E., Bernstein L., van den Brandt P.A., English D.R., Freudenheim J.L., Fuchs C.S., et al. Folate intake and risk of pancreatic cancer: Pooled analysis of prospective cohort studies. J. Natl. Cancer Inst. 2011;103:1840–1850. doi: 10.1093/jnci/djr431.
- Stolzenberg-Solomon R.Z., Hayes R.B., Horst R.L., Anderson K.E., Hollis B.W., Silverman D.T. Serum vitamin D and risk of pancreatic cancer in the prostate, lung, colorectal, and ovarian screening trial. Cancer Res. 2009;69:1439–1447. doi: 10.1158/0008-5472.CAN-08-2694.
- Ewald N., Bretzel R.G. Diabetes mellitus secondary to pancreatic diseases (Type 3c)—Are we neglecting an important disease? Eur. J. Intern. Med. 2013;24:203–206. doi: 10.1016/j.ejim.2012.12.017
- Larsson S., Wolk A. Red and processed meat consumption and risk of pancreatic cancer: A dose-response meta-analysis of prospective studies. Br. J. Cancer. 2012;106:603–607. doi: 10.1038/bjc.2011.585.
- Jiao L., Stolzenberg-Solomon R., Zimmerman T.P., Duan Z., Chen L., Kahle L., Risch A., Subar A.F., Cross A.J., Hollenbeck A., et al. Dietary consumption of advanced glycation end products and pancreatic cancer in the prospective NIH-AARP Diet and Health Study. Am. J. Clin. Nutr. 2015;101:126–134. doi: 10.3945/ajcn.114.098061
- Heinen M.M., Verhage B.A., Goldbohm R.A., van den Brandt P.A. Meat and fat intake and pancreatic cancer risk in the Netherlands Cohort Study. Int. J. Cancer. 2009;125:1118–1126. doi: 10.1002/ijc.24387.
- Ghorbani Z., Hekmatdoost A., Zinab H.E., Farrokhzad S., Rahimi R., Malekzadeh R., Pourshams A. Dietary food groups intake and cooking methods associations with pancreatic cancer: A case-control study. Indian J. Gastroenterol. 2015;34:225–232. doi: 10.1007/s12664-015-0573-4.
- Nkondjock A., Krewski D., Johnson K.C., Ghadirian P. Dietary patterns and risk of pancreatic cancer. Int. J. Cancer. 2005;114:817–823. doi: 10.1002/ijc.20800.
- Nothlings U., Wilkens L.R., Murphy S.P., Hankin J.H., Henderson B.E., Kolonel L.N. Meat and fat intake as risk factors for pancreatic cancer: The multiethnic cohort study. J. Natl. Cancer Inst. 2005;97:1458–1465. doi: 10.1093/jnci/dji292.
- Uribarri J., Cai W., Peppa M., Goodman S., Ferrucci L., Striker G., Vlassara H. Circulating glycotoxins and dietary advanced glycation endproducts: Two links to inflammatory response, oxidative stress, and aging. J. Gerontol. A Biol. Sci. Med. Sci. 2007;62:427–433. doi: 10.1093/gerona/62.4.427.
- Anderson K. E., Kadlubar F.F., Kulldorff M., Harnack L., Gross M., Lang N. P., Barber C., Rothman N., Sinha R. Dietary intake of heterocyclic amines and benzo(a)pyrene: associations with pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2005;14:2261–2265. doi: 10.1158/1055-9965.EPI-04-0514.
- Michaud D.S., Giovannucci E., Willett W.C., Colditz G.A., Fuchs C.S. Dietary meat, dairy products, fat, and cholesterol and pancreatic cancer risk in a prospective study. Am. J. Epidemiol. 2003;157:1115–1125. doi: 10.1093/aje/kwg098
- Nakamura T, Arai Y, Terada A, Kudoh K, Imamura K, Machida K, Kikuchi H, Takebe K. Dietary analysis of Japanese patients with chronic pancreatitis in stable conditions. J Gastroenterol. 1994;29:756–762.
- Setiawan VW, Pandol SJ, Porcel J, et al. Dietary Factors Reduce Risk of Acute Pancreatitis in a Large Multiethnic Cohort. Clin Gastroenterol Hepatol. 2017;15(2):257-265.e3. doi:10.1016/j.cgh.2016.08.038
- Lévy P, Mathurin P, Roqueplo A, Rueff B, Bernades P. A multidimensional case-control study of dietary, alcohol, and tobacco habits in alcoholic men with chronic pancreatitis. Pancreas. 1995;10:231–238.
- Meier RF, Beglinger C. Nutrition in pancreatic diseases. Best Pract Res Clin Gastroenterol. 2006;20(3):507-29. doi: 10.1016/j.bpg.2006.01.004. PMID: 16782526
Leave A Response